As a nutritionist working with IBS I’ve spoken to hundreds of people looking for cures for their digestive issues. If you’re searching for a solution, and tempted to get a food intolerance test then my short answer is no, don’t get an IgG test, save your money.
For a more detailed answer please read on for my take on IgG food intolerance testing for managing digestive symptoms. You can also read about my experience with a food intolerance test near the end.
Is it a food allergy or intolerance?
I know my IBS clients can feel really awful when they eat certain foods. You may get such bad bloating, gas, constipation or stomach aches that you start to think you have a food allergy.
It’s thought around 20% of adults believe they have a food allergy. In reality the number is probably lower, with Allergy UK estimating between 1-10% of adults and children have a food hypersensitivity.
But, this doesn’t mean you don’t react to food you eat! I know a lot of people have painful, uncomfortable or embarrassing digestive symptoms after meals.
Food intolerance can show up in lots of ways, and the symptoms are down to the way certain foods draw water into the intestines or ferment extra gas in some people with IBS.
These can be:
- FODMAPs causing bloating, gas and motility problems
- Lack of lactase (the enzyme to break down sugar in milk)
- Fructose malabsorption
- Non-Coeliac Gluten Sensitivity
- Histamine sensitivity
- Salicylate sensitivity
- And more!
Whilst food intolerance can be a real issue, the gut brain connection is also very important and many people with IBS have anxiety, low mood or depression.

Food allergies are different to food intolerance
A food allergy can either be an Immunoglobulin-E (IgE) mediated allergy or non-IgE allergy.
IgE is an antibody produced by your immune system when it encounters an allergen (such as the protein in egg or milk for example). The reactions are often immediate (within three hours), and can be life threatening. Non-IgE allergies involve other immune responses, and often (not always) take longer symptoms to show up (e.g. eczema flare ups).
Why get a food sensitivity test?
When people buy a food intolerance test they are normally desperate for help. You’ve tried cutting out the major culprits like dairy and gluten, but you’re STILL getting symptoms.
If this is you, you’ve probably been round and round in circles looking for the answer and feel pretty fed up.
So when someone tells you a simple at home test will tell you all the foods that are bad for you, it’s easy to see why you might go for it.
Let’s look at the actual IgG tests now.
IgG food intolerance tests – what is IgG?
Most food intolerance tests measure the antibody Immunoglobulin G (IgG). An antibody is something our immune system makes in our blood when it encounters an antigen (an antigen is something it needs to deal with, e.g. virus, or foreign bacteria).
In normal digestion the food you eat is broken down by intestinal proteolytic enzymes, and then absorbed by the cells in your gut.
It’s thought we produce IgG antibodies to foods we eat the most, which is why dairy, eggs and wheat often show up on the the tests.
Positive IgG test results are expected in normal, healthy people, as well as people with a health condition.
Are food intolerance tests accurate?
When we think about IgG testing we want to know:
- What is actually being measured – are they testing for raw or cooked chicken, raw or cooked egg?
- Is the test specific – there are four types of IgG, which subclasses of IgG measured?
- Whether the same result could be reproduced in different labs?
- Does this marker actually have an effect on your health – i.e. if IgG is high does it correlate to your symptoms?
There is no regulation of IgG tests so it’s difficult to be sure how good the lab is. The half life of IgG antibodies is around 23 days, but they could last much longer.
What does a high IgG food intolerance result show?
If you have a raised level of IgG4 antibody to a food this indicates that you’ve eaten that food in the last 60 days. The presence of IgG is your immune system’s way of handling an alien protein. It doesn’t mean it should be treated as a sign of hypersensitivity. IgG is a marker of immune tolerance.
Research study – increasing IgG = increasing tolerance (2009)
- When patients have an IgE allergy sometimes a medically controlled research project will try to see if tiny amounts of the allergen can increase their permanent tolerance to foods such as milk or peanuts.
- These experiments actually saw increases in patients’ IgG4 levels to those foods. In fact one study measuring oral immunotherapy to peanuts in people with a peanut allergy showed IgG increased as they were exposed to of tiny amounts of peanut and IgE decreased. The study goes so far as to say:
Elevated IgG is associated with immune tolerance, not intolerance
Increased levels of specific IgG4, with or without decreased IgE, have been associated with:
- successful immunotherapy,
- lower levels of symptoms in parasite infections,
- transient rather than persistent milk allergy,
- and the apparent protective effect of high levels of cat allergen exposure.
Experts say the results of the IgG tests are hard to interpret for both medical practitioners and patients themselves because the test shows IgG antibodies against foods often eaten by the patient.
So what does it all mean?

Do raised food intolerance IgG levels affect IBS?
Let’s have a look at some studies:
No significant correlation between symptom severity and IgG levels in patients with IBS (Zuo, 2007)
- Serum IgG and IgE antibody titres to 14 common foods including beef, chicken, codfish, corn, crab, eggs, mushroom, milk, pork, rice, shrimp, soybean, tomatoes and wheat were analysed for 37 IBS patients, 28 patients with functional dyspepsia and 20 healthy controls. Symptoms were also measured.
- IgG levels were shown to be higher in those patients with IBS or functional dyspepsia but no significant correlation was seen between symptom severity and IgG levels in patients with IBS or functional dyspepsia
Removal of typical IBS trigger foods = improvement in symptoms (Atkinson 2004)
- This study from 2004 gave patients a sham diet, or a diet removing the foods which had shown up a higher IgG result in a food intolerance test. The IgG group showed a 10% greater reduction in food related digestive symptoms in the food intolerance diet, compared to the sham diet.
- However, large proportions of the treatment group removed common high FODMAP foods which are often removed as part of an IBS diet protocol. The sham diet group continued to eat wheat, cow’s milk, peas, cashew nuts and yeast (see table 2 in the study link).
- This is one of the reasons you might feel better after an IgG led elimination diet – removing common dietary triggers, as well as adding new foods into your diet, can be transformational in some cases of IBS.
High IgG not associated with skin symptoms (Antico et al, 2010)
- Antico & colleagues in 2010 found in 45 people (62%) were IgG4 positive for a number of foods, mainly egg, milk, casein and wheat. All patients took skin tests, measurements of IgE and IgG4, open oral provocation challenges with foods for which IgG were detected, and double-blind placebo-controlled food challenges with foods for which the open food challenges were positive.
- In the food challenge trial, none of the 45 in whom IgG4 was found showed intolerance to the foods for which IgG4 was detected.
- In conclusion, the authors stated that measuring IgG4 in adult patients is not useful clinically in the diagnosis of food allergy or intolerance.
Absence of positive evidence
As well as these studies which don’t show support for IgG food tests we are missing any positive research. For example, there are no studies comparing a standard IBS intervention diet, such as a low FODMAP diet, to an IgG test elimination diet.
The European Academy of Allergy and Clinical Immunology, EAACI, Task Force Report found – “Testing for IgG4 against foods is not recommended as a diagnostic tool”
What is the issue with food intolerance testing?
The main problem with incorrectly diagnosing a food intolerance is that you don’t actually uncover the real reason for your symptoms. This could delay you getting the help you need.
And secondly, a dodgy restrictive diet means you’re missing out on eating a lot of food that could actually be really good for you. This could be reducing your diet variety, and potentially creating more anxiety around your food.
I see clients all the time who have concerns about eating certain foods that don’t actually cause a problem when we bring them back in again.
If you’ve been avoiding certain foods for a long time you might want to read my tips for reintroducing foods after an elimination diet.
What about other food intolerance tests – Vega test and kinesiology
These kinds of tests don’t have any research to back them up and I don’t recommend using these:
- vega testing – claims to detect food intolerance by measuring changes in your electromagnetic field
- kinesiology testing – claims work by studying energy changes in your muscle responses to food exposure (sometimes diluted in a glass jar)
How to check if you have food intolerance
Start keeping a diet diary to measure how you’re reacting to foods over time. (if you need any guidance on using a food diary see my Benefits of a Diet Diary for IBS here
Don’t just look at your food, but also consider your stress levels, sleep, and exercise routine. Monitor your bowel movements, mood and any other relevant symptoms (e.g. headaches, eczema)
Look for patterns in how you ate, as well as what you eat. Think about when you rushed to eat a meal or when you ate feeling really stressed.
The way you eat can have a big impact on digestive symptoms.
What happened when I took a food intolerance test?
Not much!
When I was training to become a nutritional therapist I was offered a free food intolerance test. I was so curious about what it might tell me I tried it out.
My test came back with seven foods with elevated IgG antibodies, and five medium level IgG levels. At the time I didn’t have any symptoms, digestive or otherwise, that I was hoping to address. I still tried a few weeks of avoiding the key seven ‘red foods’. I didn’t notice anything different about my health during this period.

These were foods I was eating a lot of at the time which matches the assessments above that IgG is produced when we eat foods.
I definitely didn’t eat oyesters though so I don’t know where this came from.
I did try avoiding eggs and almonds for a while and started worrying that they weren’t good for me after all. And this is part of the problem, encouraging people to give up foods that don’t cause an issue can lead to reduced nutrient intake, and fear of food.
In summary – IgG food intolerance tests aren’t worth the money
If you have an experience of IgG food intolerance testing I’d love to hear your comments below.

IBS Nutritionist
Hi I'm Anna Mapson, registered Nutritional Therapist.
I help people with IBS and SIBO get control of unpredictable gut symptoms to find long term relief from painful and embarrassing IBS without restrictive dieting.
I can help you to:
- understand your digestion better, so you recognise your triggers
- eat a well balanced diet, with tasty meals that are simple to prepare
- reintroduce your trigger foods so you can get back to enjoying food again
Find more about my 3 month 1:1 Gut Reset programme
Low FODMAP Vegetables for IBS relief
Confused about which vegetables are low FODMAP? Dealing with IBS can throw some serious curveballs into your meal planning, right? But don't worry, you can still include lots of veg in your meals. I'm here to dish out some tasty tips on navigating the low FODMAP diet...
IBS and Coeliac Disease: A Guide to Understanding & Diagnosis
Are you confused about IBS and coeliac disease? Maybe you feel better without gluten in your diet, but you're not sure whether you've been tested for coeliac disease or not. The cross over between IBS and coeliac disease 1 in 4 people are misdiagnosed with IBS when...
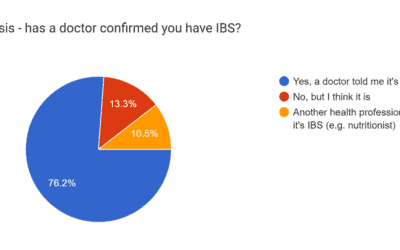
The impact of IBS on daily life
The struggles of IBS: A new survey reveals the profound impact on daily life. I ran a survey with my audience about the impact of IBS, and the way Irritable Bowel Syndrome (IBS) affects your day-to-day lives is really clear. I already knew from my work with clients...


Hi, I have IBS-C , and recently Diagnosed with Diverticulosis. I have tried everything u can think of to help my issues.
Hi there, that sounds like you’re dealing with quite a lot, would you like to arrange a time to speak to me about the Gut Reset and working with me 1:1 on your issues? Please contact me https://www.goodnessme-nutrition.com/contact/ to arrange a time to talk through what you’re looking for, Anna